You’ve probably seen news about the nation’s behavioral health crisis. Due to a heightened demand for services and shortage of mental health providers, more and more people have an unmet mental health need.
This imbalance also translates to an increased cost of behavioral healthcare nationwide. In 2020, the US spent $280B on mental health services, and for payers, behavioral health services claims continue to increase at an alarming rate. At CareFirst BlueCross BlueShield (CareFirst), this increase has been more than 20% since 2019.
There is a clear need to develop solutions to optimize what is currently available. We can find ways to do this with advancements in telehealth and spending venture capital wisely.
Many behavioral health solutions operate by supporting Primary Care Providers (PCPs). PCPs are the first touchpoint for most patients’ healthcare journey but are often ill-equipped to address behavioral health needs since it’s not their traditional focus.
PCPs need a model where they can leverage patient relationships while engaging with behavioral health experts to get them high-quality mental health care. This is where collaborative care comes into play.
The Collaborative Care Model (CoCM) has been around for over 20 years, helping PCPs diagnose and support their patients’ behavioral health needs.
This model was standardized in 2011 by the University of Washington, which found through 90 randomized control trials that CoCM has proved cost-effective and decreased the time to remission of depression. 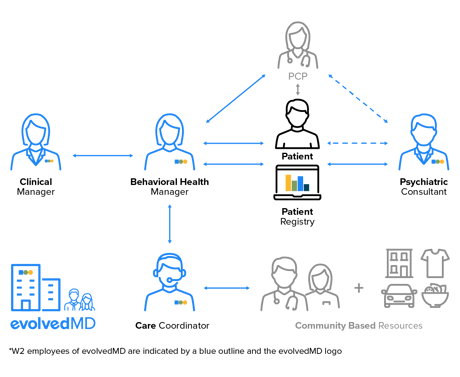
In this collaborative care market, solutions have largely clustered around two main approaches: virtual-only and hybrid.
With virtual-only methods, patients fall through the cracks, especially those with serious conditions such as paranoia and hoarderism, or those who feel more comfortable with in-person interactions.
This makes the hybrid model, which optimizes virtual and in-person modalities, the preferential way to provide care. We believe a hybrid solution that uses an in-person first model and embeds therapists into practices will offer the most effective, seamless patient treatment.
A great example of this approach in action is evolvedMD, a collaborative care company based in Scottsdale, Arizona uses a hybrid approach to improve access, engagement and integration of behavioral health into physical healthcare.
That’s why at Healthworx Ventures, we are thrilled to support Steve Biljan and Erik Osland, the founders of evolvedMD, by investing in their Series A-prime.
With an experienced founding team and a proven business model, there were countless reasons to invest in evolvedMD, though their results speak for themselves: a ten times faster time to remission of depression than industry standard. And, their model gets patients care without over-exerting behavioral health professionals.
More thoughtful innovations like this are critical, which is why we’re committed to investing in more behavioral health solutions that work for both patients and providers.
...
Visit the Healthworx Ventures team page if you’re interested in connecting with them or learning more.